Comparison of Histopathology and Mammography for breast lesions. Retrospective study of 250 cases in Srinagarind Hospital, Khon Kaen, Thailand.
Chotiyano A1, Srinakarin J2, Triamwittayanont T1, Wongsiri T1, Koonmee S1.
1Department of Pathology and 2Department of Radiology, Faculty of Medicine,
Khon Kaen University,Thailand.
Received: 16 July 2013; Accepted: 21 September 2013.
ABSTRACT
Purpose: To assess the pathologic outcome of BI-RADS mammographic classification and the success of stereotactic biopsy for such lesions.
Materials and Methods: A retrospective study of 250 consecutive patients undergoing breast biopsy for mammographic abnormalities from January 2004 to December 2008 at the Breast Diagnostic Center, Faculty of Medicine of the Srinagarind Hospital was performed to identify biopsies done for indeterminate microcalcifications and breast lesions. Specimens showed normal breast tissue, fibroadenosis, fibrocystic changes, fibroadenoma, ductal carcinoma in situ, lobular carcinoma in situ, invasive ductal carcinoma, invasive lobular carcinoma, tubular carcinoma, mucinous carcinoma, medullary carcinoma and diffuse large B-cell lymphoma. They were identified and reviewed by one pathologist. The BI-RADS mammographic classification data was compared with histopathological data. Continuous variables were summarized as mean (standard deviation) or median (range) as appropriate. Categorical variables were summarized as counts and percentages. Associations between histological findings and patterns of radiographic characteristics were determined using logistic regression analysis. These associations were reported as odds ratios. Statistical significance was defined as a p-value of 0.05 or less. All statistical analyses were performed using Stata v. 7 (Stata Corp, College Drive, Texas, USA).
Results: From the 424 studied women, the 250 (58.9%) were categorized as BI-RADS category. Among these, 9 malignant lesions were seen in BI-RADS category 0, 5 in BI-RADS category 2, 11 in BI-RADS category 3, 52 in BI-RADS category 4, 46 cases in BI-RADS category 5 and 2 cases in BI-RADS category 6. Positive predictive value (PPV) of the BI-RADS category 5 criteria in diagnosing breast cancer in the present study was 85% (46 of 54 patients). This PPV was compatible with the PPV advocated by the American Cancer Research (ACR), which proposed a PPV of at least 95%, and that of other published studies which ranged from 80-97%.
INTRODUCTION
Evaluation of calcifications in breast lesions is a major assessment criterion for breast mammography. The morphology and distribution of the calcifications are related to the histology of the lesions. Radiologically, calcifications can be divided into: benign; intermediate concern; and higher probability of malignancy according to the morphology. Different pathological entities may give rise to different calcifications. Fibrocystic changes may give rise to milk of calcium or teacup type calcifications, or small calcifications occurring in a cluster1. Fibroadenoma may be associated with large popcorn-like calcifications, and sclerosing adenosis may have fine, punctuate or granular calcifications 6. Fat necrosis may give rise to eggshell calcifica-tions1. Precursor malignant lesions give rise to benign and indeterminate type calcifications, and may occasionally be associated with malignant type calcifications. For malignant lesions, ductal carcinoma in situ and invasive ductal carcinoma may be associated with large irregular, rod or V shaped, pleomorphic or branching type calcifications that follow the distribution of the ducts2, 6 7 10, 15, 16, 18, 19. Furthermore, analysis of the characteristics of the calcifications may help to predict the tumour size, grade, and invasion.
In 1992, the American College of Radiology (ACR) formed Breast Imaging Reporting and Data system (BI-RADS) to standardize mammographic interpretation3. The fourth edition of BI-RADS was introduced in 2003 and proposed a BI-RADS system for the ultrasound (US)3. Details of the BIRADS for mammography and US are as follows: Category 0: Incomplete assessment, additional imaging evaluation and/or prior mammograms for comparison are needed. Category 1: Negative, annual screening mammogram is recommended. Category 2: Benign finding(s), annual screening mammogram is recommended. Category 3: Probable benign finding, initial short-interval follow up is suggested. Category 4: Suspicious abnormality, biopsy should be considered. Category 5: Highly suggestive of malignancy, appropriate action should be taken. Category 6: Known biopsy-proven malignancy, appropriate action should be taken2, 3 20. BI-RADS category was created to format mammographic and US interpretation among radiologists, to standardize assessment of the findings, to communicate with the referring physicians and to recommend appropriate care according to imaging findings.
The positive predictive value of a biopsy positive for malignancy increases from less than 2% for BI-RADS category 3 mammograms to 2330% for category 4 mammograms and to 95% for |category 5 mammograms20. Specific mammographic findings with the highest positive predictive value of malignancy include masses with spiculated margins and/or irregular shape, as well as calcifications with linear morphology and/or segmental distribution.
The purposes of the present study were to determine the positive predictive value (PPV) of mammograms and ultrasonography categorized as BI-RADS category 3, and 5 in the diagnosis of breast cancer in the present center and to determine the correlation between clinical, mammographic and ultrasound findings with the pathological diagnosis of breast cancer.
MATERIALS AND METHODS
From January 2004 to December 2008, 424 women, who underwent screening and diagnostic mammogram at the Breast Diagnostic Center, Faculty of Medicine, Srinagarind Hospital were studied. 174 patients did not have histopathological records at Srinagarind Hospital and were excluded from the study. Therefore, two hundred and fifty patients were enrolled. Clinical information, mam-mographic, ultrasound findings and histopathologi-cal diagnoses were retrospectively reviewed.
The interpretation of mammogram findings included reports on general tissue features and limits of assessment. For each lesion, clock-face location and distance from the nipple were noted. The lesion was characterized using BI-RADS mammogram descriptors of mass margin; circumscribed, obscured, microlobulated, ill-defined/indistinct, or spiculated, shape; oval, round, lobular or irregular3, 4, orientation; parallel or not parallel to the skin, matrix echogenicity and homogeneity; anechoic, hypoechoic or hyperechoic; homogeneous or heterogeneous and attenuation; indifferent, shadowing or enhancement. Additionally, any associated findings (e.g. architectural distortion) or axillary lymphadenopathy were noted.
The needle core biopsy or Bard’s biopsy was performed. Pathological diagnosis was obtained from pathologic reports from the Department of Pathology, Faculty of Medicine and these were compared with mammogram and ultrasound findings.
The patients’ data, medical history, breast ultrasound findings and histological diagnosis of each case were stored in an electronic database and compared with the allocated mammogram BI-RADS category. Lesions initially diagnosed by core needle biopsy as atypia, malignant or having discordant imaging and histology underwent surgical excision. For discordant and malignant lesions, final histological diagnosis was based on excisional biopsy results. Unfortunately, mammography was not performed in all of our patients and mammography reports were not included in our database; therefore, a direct comparison of BI-RADS categories of ultrasound and mammography was not possible in this study.
Continuous variables were summarized as mean, standard deviation or median range) as appropriate. Categorical variables were summarized as counts and percentages. Associations between histologic findings of malignancy and patients or radiographic characteristics were determined using logistic regression analysis. These associations were reported as odds ratios. Statistical significance was defined as a p-value of 0.05 or less. Statistical analyses were performed using Stata v. 7 (Stata Corp, College Drive, Texas, USA).
RESULT
The age of the 250 patients ranged from 13 to 82 years (mean 48.16 years). The lesions were found in the right breast (117 cases) more than the left (114 cases) and 19 cases of bilateral lesions. The most common site of the lesion was at the upper outer quadrant.
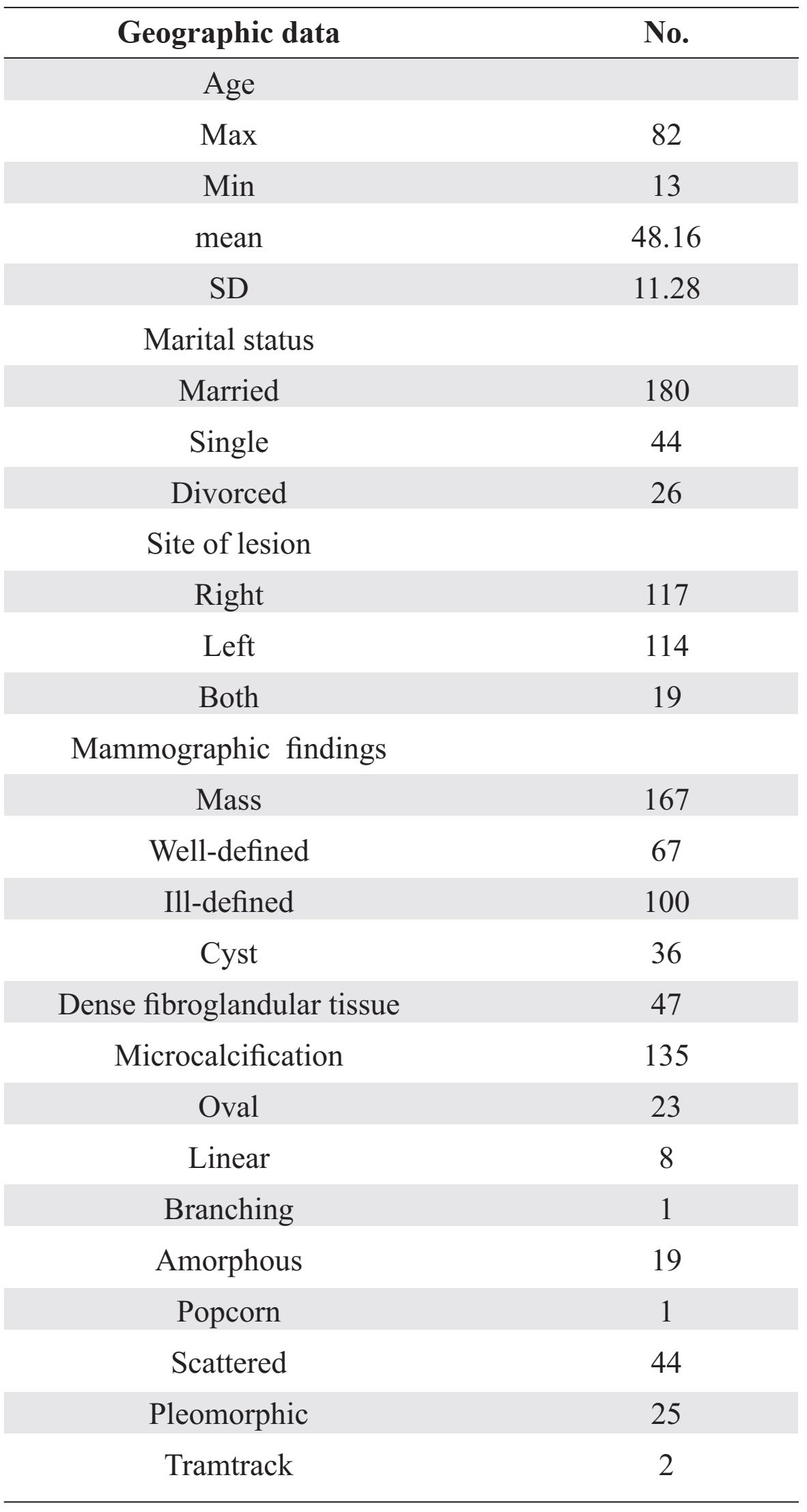
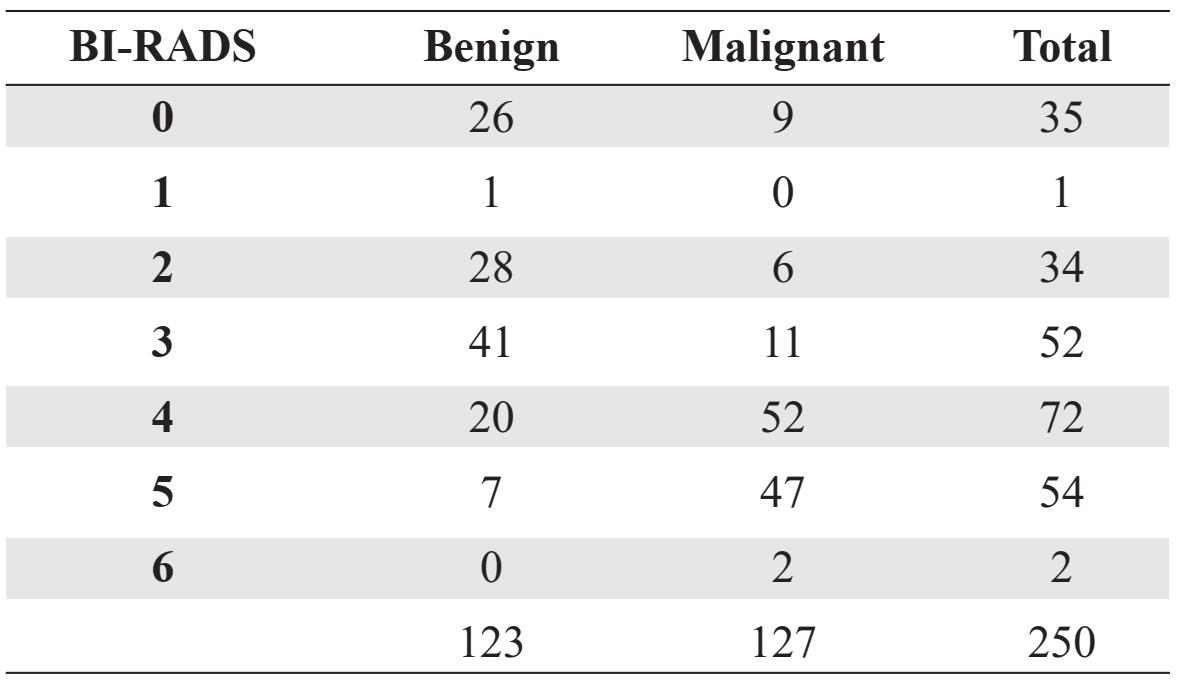
Mammographic findings showed: mass lesion (167 cases, 66.8%), cystic lesion (36 cases, 14.4%), and dense fibroglandular tissue (47 cases, 18.8%). The microcalcifications were detected in 135 cases (54%) and classified as oval, linear, amorphous, branching, popcorn, pleomorphic, tram track and scattered (Table 1). The mammographic BI-RADS classification was classified and shown as following; 35 cases of category 0, 1 case of category 1, 34 cases of category 2, 52 cases of category 3, 72 cases of category 4 and 54 cases of category 5 and 2 cases of category 6. From these 250 specimens malignant lesions were found in 9 cases (3.6 %) of BI-RADS category 0, 6 cases (2.4%) of category 2, 11cases (4.4%) of category 3, 52cases (20.8%) of category 4, 47 cases (18.8%) of category 5 and 2 cases (0.8%) of category 6 (Table 2).
Table 1 Geographic data and mammographic data findings.
The common malignant lesion was invasive ductal carcinoma (112 cases, 44.8%), followed by ductal carcinoma in situ (14 cases, 5.6%) and invasive lobular carcinoma (4 cases, 1.6%); there were 2 cases of colloid carcinoma and papillary carcinoma and 1 case of tubular carcinoma and diffuse large B-cell lymphoma.
The common benign lesion was fibrocystic change (45 cases, 18%), followed by fibroadenoma (21 cases, 8.4%), ductal epithelial hyperplasia (17 cases, 6.8%), fibrosis (12 cases, 4.8%), fibroadenosis (15 cases, 6%) and unremarkable breast tissue (4 cases, 1.6%).
Table 2 Mammographic BI-RADS classification and histologic findings
Microcalcifications in invasive ductal carcinoma were detected in 59 cases (52.6% of invasive ductal carcinoma) and showed scattered shape in 27 cases, pleomorphic shape 12 cases, amorphous 9 cases, rod shape 4 cases, round shape 6 cases and 1 case of tam-track shape.
The mammographic findings of invasive ductal carcinoma showed mass with microcalcifications and architectural distortion in 49 cases (48% of invasive ductal carcinoma cases), mass without microcalcification 33 cases (32%), dense breast tissue with microcalcification 12 cases (12%), dense breast tissue without microcalcification 5 cases (5%) and mass with cystic lesion and without microcalcification 3 cases (3%).
The mammographic findings of fibrocystic change showed cystic lesion without microcalcification in 11 cases (24.4% of fibrocystic change cases), mass without microcalcification 9 cases (20%), mass with microcalcifications 8 cases (17.7%), dense breast tissue with microcalcifications 6 cases (13.3%), dense breast tissue without microcalcification 5 cases (11.1%), mass with cystic lesion and microcalcifications 2 cases (4.4%) and mass with cystic lesion without microcalcification 1 case (2.2%).
The sensitivity and specificity of mam-mographic screening of breast cancer compared between BI-RADS category 1 (which means that the mammogram was negative) and BI-RADS category 5 (which means that mammogram results were highly suspicious with a 95% chance of breast cancer) were 100% of sensitivity but only 11.1% of specificity.
The positive predictive values, prevalence of breast cancer and pretest odd ratio of BI-RADS category 3 and 5 lesions were as following; 0.21 and 0.87, 4.4% and 18.8%, 0.046 and 0.23, respectively.
There were 7 lesions (2.8%) categorized as BI-RADS category 5 but the histologic lesions were benign (false positive) (Table 3), while 6 and 9 lesions previously categorized as BI-RADS category 2 and 0, respectively, were malignant lesions (false negative) (Table 4 and 5). An example of such cases, a 54-year-old woman with mammographic screening and false positive mammography is shown in figure 1.
Table 3 The mammographic, sonographic findi ngs, microcalcification patterns and histologic findings of 7 false positive BI-RADS category 5 patients.
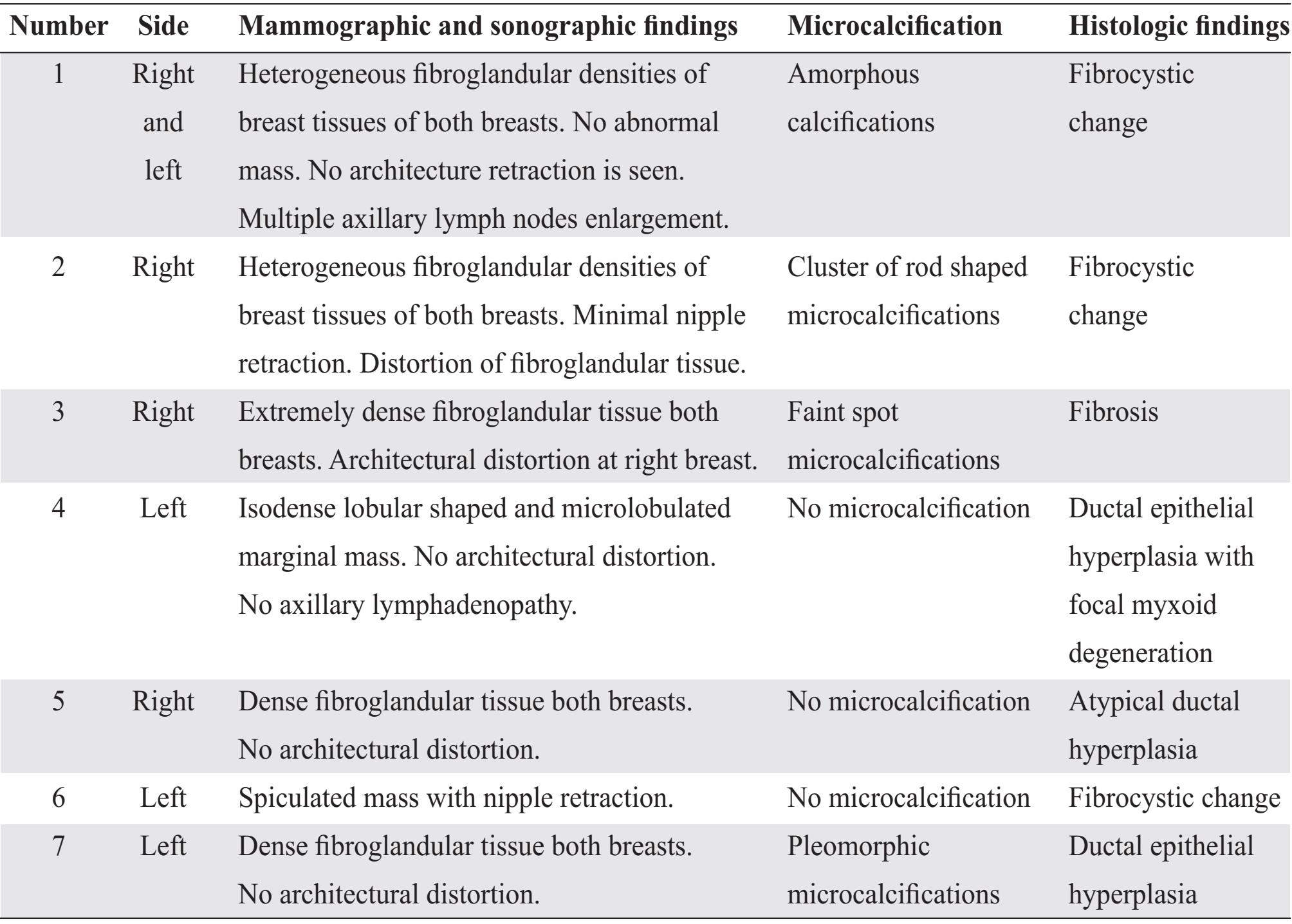
Table 4 The mammographic, sonographic findings, microcalcification patterns and histologic findings of 6 false negative BI-RADS category 2 patients.
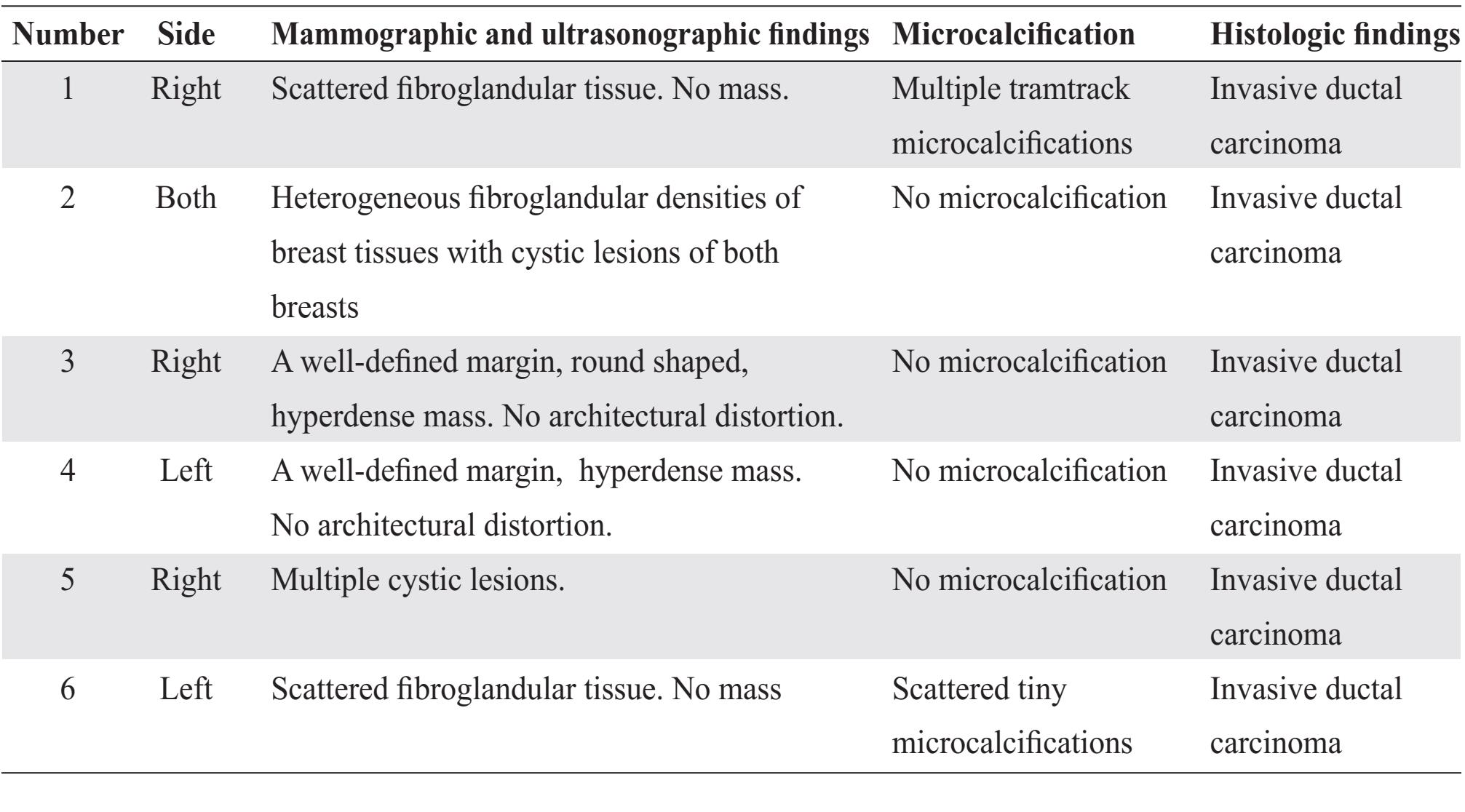
Table 5 The mammographic, sonographic findings, microcalcification patterns and histologic findings of 9 false negative BI-RADS category 0 patients.
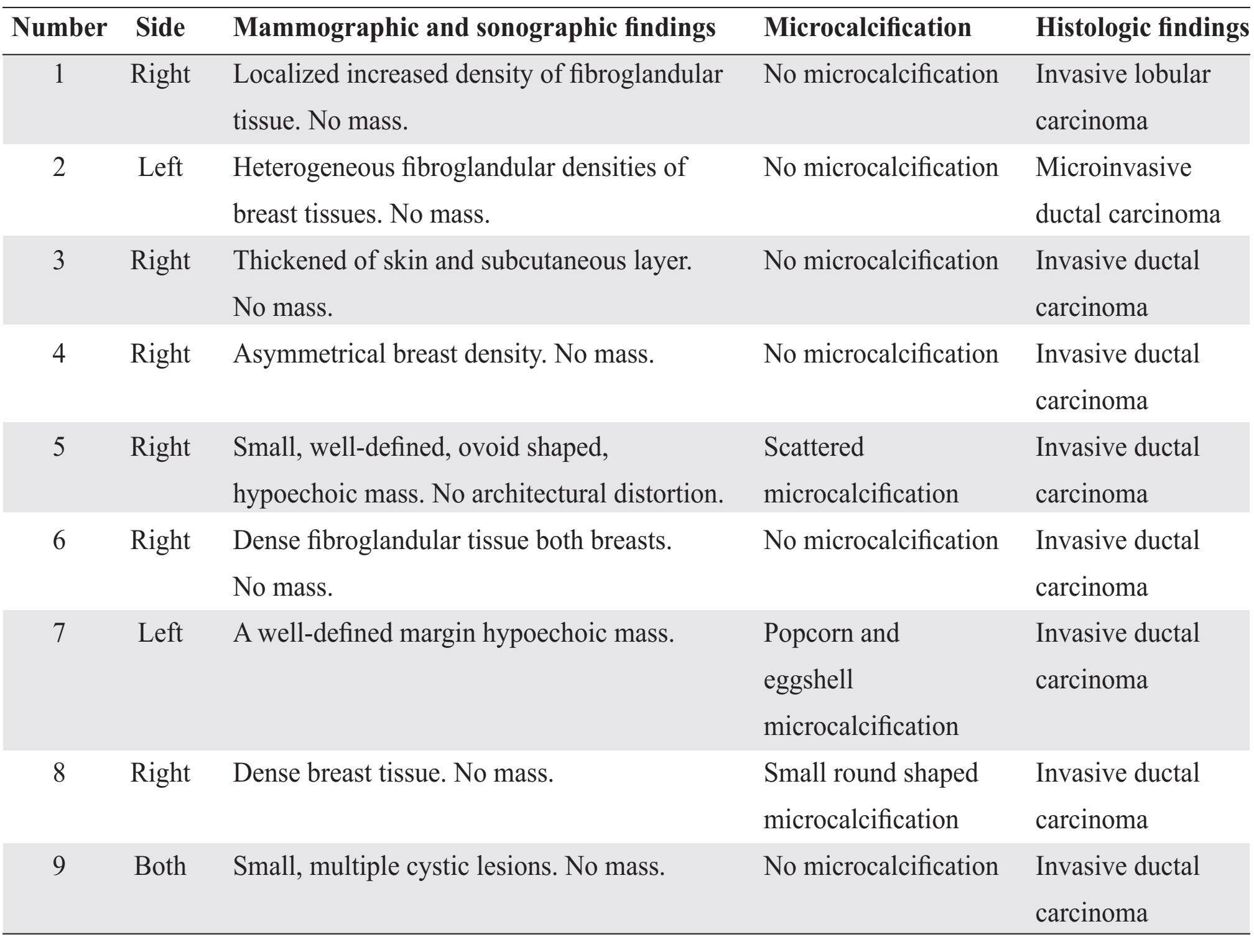
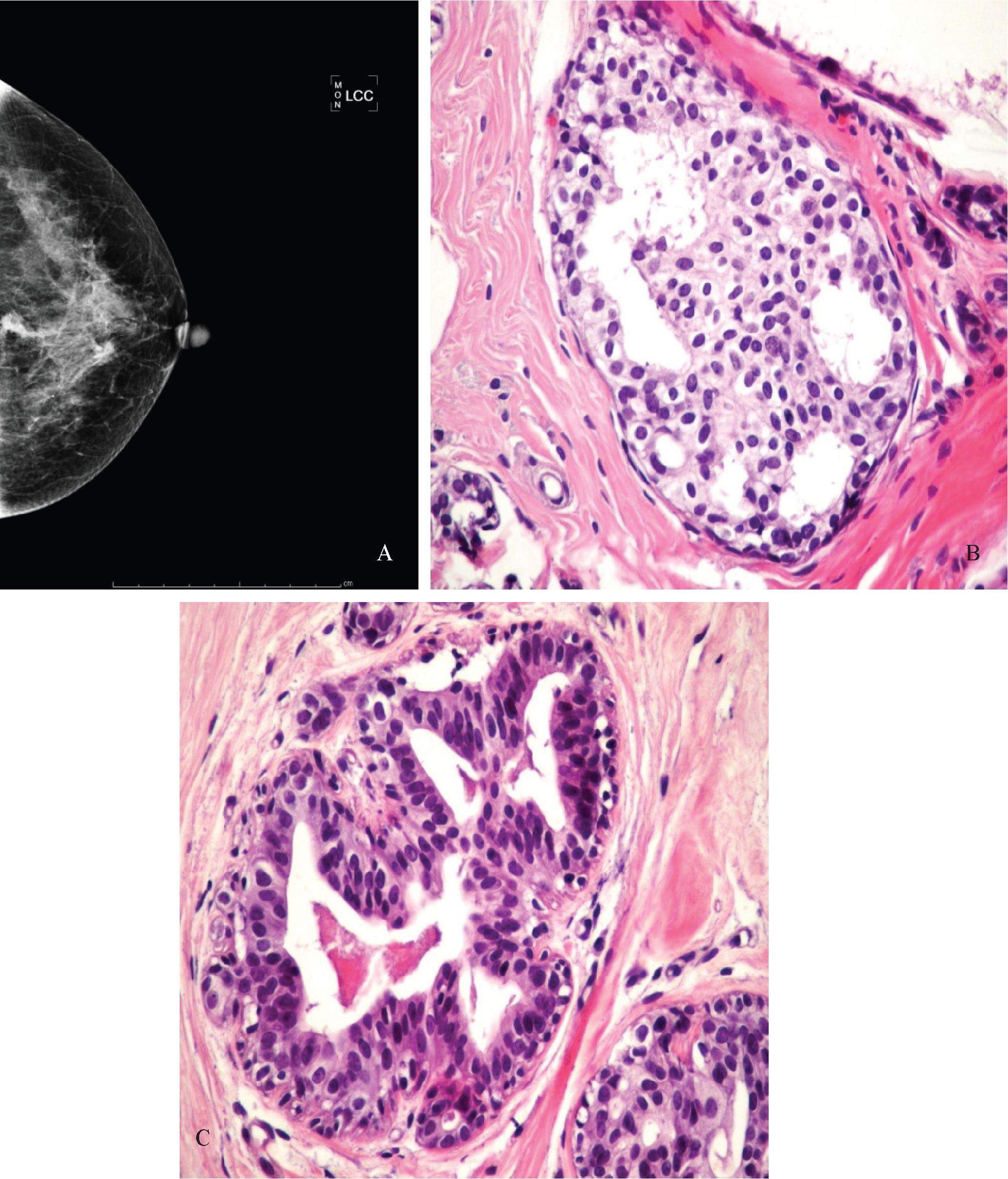
Figure 1 A 54-year-old female, for screening: A; Mammogram findings of the left breast on CC view: heterogeneous fibroglandular tissue. No architectural distortion. There is an irregular mass contains pleomorphic calcification located at mid part of the left breast and categorized in BI-RADS category 5 (arrow). B; Histological findings show an increase in epithelial layer lining which distends the terminal ducts and ductules. The epithelial proliferation forms solid masses filling the lumen. Individual cell borders are inconspicuous so that the cell mass has a syncytial appearance. Nuclear spacing is uneven leading to overcrowding and nuclear overlap in areas and nucleoli are inconspicuous. Oval nuclei are arranged parallel to the long axis of the ridge. (40x) and C; microcalcifications present in the lumens. (40x)
DISCUSSION
Mammographic detection of calcification remains the hallmark of detection of non-palpable breast malignancy. In general, calcifications which are large (over 0.5 mm. in diameter), smooth, round, dense, scattered over a large area, bilateral or associated with some benign process, are classified as benign. Malignant calcifications show scattered, pleomorphic or linear morphology. Clustered calcifications (5 calcifications in 1 ml of tissue volume) are pleomorphic and calcifications /or punctate (tiny dots, 1 mm, resembling salt)6. Linear calcifications, including branching, are derived from casts of the ducts, particularly those with necrotic content. Stability over time should be considered: static calcifications are considered benign, and new or increased calcifications must be viewed with suspicion.
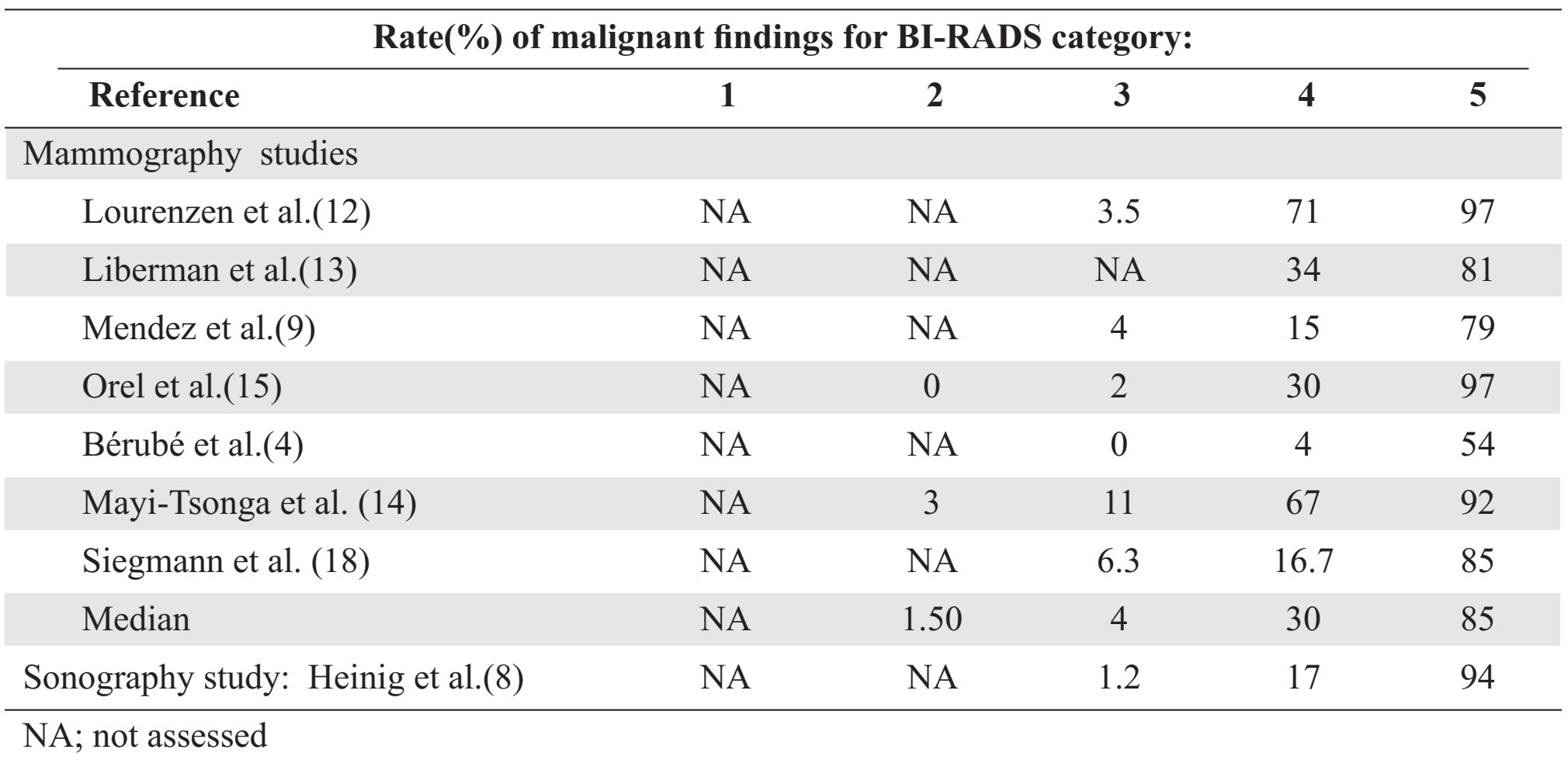
Heinig J et al.8 reviewed the previous studies and showed increased incidence of malignant lesion in BI-RADS category (Table 6).
Table 6 Incidence of malignancy determined by mammography in previous studies and by sonography in Heinig J et al. (8) study according to ultrasound breast imaging reporting and data system (BI-RADS) category
Mammogram and ultrasound are recommended adjunctive diagnostic tools for screening palpable and non-palpable abnormalities of the breast. They are also effective for further mammo-graphic and clinical evaluation. The predominant mammographic finding of breast cancer is the presence of mass, typically presented as irregular shape, ill-defined or spiculated margin, and sometimes displayed as high density lesion on imaging of mammography. Approximately 60% of cases, the mass usually associated with malignant calcification. The frequency of lesions categorized in BI-RADS category 5 reported in previous studies varied due to the prevalence of various cancerous types found in each of them. According to Orel et al., the most compatible histopathological lesion for breast cancer is the presence of mass15, and the mammographic hallmark of ductal carcinoma in situ (DCIS) is the presence of calcification. The latter finding might be the only positive finding in 70-80% of cases.
Tan et al. also mentioned that microcalcification was the most frequently lesion reported among various studies and DCIS was also the common malignancy finding10.
From this study, the positive predictive value (PPV) of the BI-RADS category 5 for diagnosing breast cancer was 85% (46 of 54 patients). It was compatible with at least 95% of PPV, suggested by the American Cancer Research (ACR), and also supported by others studies, which suggested PPV ranges from 80-97% 20. From Tan et al. study10, which both mammography and ultrasound techniques were used in studying method, PPV was reported as 84%. So, from these mentioned evidences, suggested mammography and ultrasound were useful for better prediction of breast cancer, especially in highly suspicious lesions.
This study showed that 7 patients (2.8%), who presented with lesions initially categorized in BI-RADS category 5, displayed benign histological diagnosis. Fibrocystic change was the predominated benign lesion, while the second most common was fibroadenoma. The most common mammographic and ultrasonographic findings in false positive lesions were as following: dense fibroglandular tissues, absence of abnormal mass with architectural distortion, and even no microcalcification. The microcalcification patterns showed amorphous, pleomorphic, scattered and rod shape.
Although there were 6 and 9 patients categorized in BI-RADS category 2 and 0, respectively, malignant lesions were still subsequently found from biopsies. Invasive ductal carcinoma was the predominant malignant lesion found in false negative lesions. From mammographic and ultrasonographic results, we found that there was also the significant lesion presented in false negative group; the dense fibroglandular tissues, in which sometimes they were accompanied by abnormal mass or microcalcifications. And in microcalcified lesions, there were various patterns presented as following; scattered, popcorn, eggshell, tram track and round-shaped pattern. The most important problem of detecting malignant lesions in mam-mographic and ultrasonographic was the variety of tissue densities distributed among breast regions14. Other problems were location of lesions, tissue background and diagnostic imaging techniques.
Invasive breast cancers usually associated with microcalcifications2, 7 10, 15, 16, 18, 19. In which the lesions appeared as masses containing calcifications, detectable on mammogram, indicating the most possible diagnosis of breast cancers. In this study, we demonstrated pleomorphic calcifications within mass and heterogeneity of surrounding tissue, in which malignant lesion should be suspected. Benign calcifications as the result of fibrocystic change or benign proliferative disorders tend to be surrounded by hyperechoic tissues. Anyways, in this study, the limitation of detecting lesion on ultrasonography was affected by various radiologists experience.
Depending on microcalcification on detecting cancerous lesion alone, had relatively low chance of detecting false negative; spiculated masses were the common feature in breast cancer. The ill-defined masses could increase the risk of mistaking ones as false negative among cancerous lesions. From the mammogram of lower retroglan-dular region of the breast in which there were more adipose tissues deposition than other regions, it appeared that false negative results were more likely to be reported than true positive ones. So, this information suggests that we should be precautious about this region by performing mammography on each screening examination.
ACKNOWLEDGEMENTS
The authors wish to thank Dr.Thaomani Ruaysoongnem and Dr.Chongkon Klungsombat, resident of Department of Pathology and Department of Radiology, respectively for sharing resources.
REFERENCES
1. G M Tse, P-H Tan, A L M Pang, A P Y Tang, H S Cheung. Calcification in breast lesions: pathologists’ perspective. J Clin Pathology 2008; 61: 145-151.
2. Al-Nafussi AI. and Hughes DE. Histological Diagnosis of Tumor by Pattern Analysis. New York:Oxford University Press Inc, 2001: 127157.
3. American College of Radiology. BI-RADS: mammography. In: Breast Imaging Reporting and Data System: BI-RADS Atlas. 4th ed. Reston: American College of Radiology, 2003.
4. Berube M, Curpen B, Ugolini P, Lalonde L, Ouimet-Oliva D. Level of suspicion of a mam-mographic lesion: use of features defined by BI-RADS lexicon and correlation with large-core breast biopsy. Can Assoc Radiol J 1998; 49:223-228.
5. Boo-Kyung Han, Yeon Hyeon Choe, Young-Hyeh Ko, Seok-Jin Nam, Jung-Han Kim,Jung-Hyun Yang. Stereotactic Core-Needle Biopsy of Non-Mass Calcifications: Outcome and Accuracy at Long-Term Follow-Up. Korean J Radiol 2003; 4:217-223.
6. Filipe MI. and Lake BD. Histochemistry in Pathology. 2nd ed. London:Churchill Livingstone, 1990: 335-354.
7. Heinig J. ,Witteler R. ,Schmitz R., Kiesell., Steinhard J. Accuracy of classification of breast ultrasound findings based on criteria used for BI-RADS. Ultrasound Obstet Gynecol 2008; 32: 573-578.
8. Mendez A, Cabanillas F, Echenique M, Malek-shamran K, Perez I, Ramos E. Mammographic features and correlation with biopsy findings using 11-gauge stereotactic vacuum-assisted breast biopsy (SVABB). Ann Oncol 2004; 15: 450-454.
9. Kok-Yan Tan, Su-Ming Tan, Siew-Hwa Chiang, Andrew Tan, Chee-Keong Chong, Khoon-Hean Tay. Breast specimen ultrasound and Mammography in the prediction of tumor free margins. Anz J of Surgery 2006; 76: 1064-1067.
10. Kumar V, Cotran RS and Robbins SL. Basic Pathology. 5th ed. Philadelphia:W.B. Sauders Co, 1992: 631-641.
11. Lorenzen J, Wedel AK, Lisboa BW, Loning T, Adam G. Diagnostic mammography and sonography: concordance of the breast imaging reporting assessments and final clinical outcome. Rofo 2005;177:1545-1551.
12. Liberman L, Abramson AF, Squires FB, Glass-man JR, Morris EA, Dershaw DD. The Breast Imaging Reporting and Data System: positive predictive value of mammographic features and final assessment categories. AJR Am J Roentgenol 1998; 171: 35-40.
13. Mayi-Tsonga S, Meye JF, Ngou-Mve-Ngou JP, Mendome G, Mounanga M. Nonpalpable breast lesions: correlation of the BI-RADS classification and histologic findings. Sante 2006; 16: 179-183.
14. Orel SG, Kay N, Reynolds C, Sullivan DC. BI-RADS categorization as a predictor of malignancy. Radiology 1999; 211: 845-850.
15. Rosai J. Ackerman’s Surgical Pathology. 8th ed. Missouri:Mosby-Year Book Inc, 1996: 15651660.
16. Rubin E, Gorstein F, Rubin R, Schwarting R and Strayer D. Rubin’s Pathology: Clinico-pathologic Foundations of Medicine. 4th ed. Maryland:RR Donnelley-Willard, 2004: 996.
17. Siegmann KC, Wersebe A, Fischmann A, Fersis N, Vogel U, Claussen CD, M" uller-Schimpfle M. Stereotactic vacuum-assisted breast biopsy-success, histologic accuracy, patient acceptance and optimizing the BI-RADS-correlated indication. Rofo 2003;175:99-104.
18. Standler N. and Klionsky B. Cases in Pathology. In: A clinical approach for students. London: Churchill Livingstone, 1992: 207-210.
19. Tavassoli FA. and Devilee P. WHO Classification of tumours, Pathology & Genetic : Tumour of the breast and The female genital organ. Lyon:IARC Press, 2003: 9-110.
20. Wiratkapun C, Lertsithichai P, Wibulpholprasert B. Positive Predictive Value of Breast Cancer in the Lesions Categorized as BI-RADS Category 5. J Med Assoc Thai 2006; 89(8): 1253-1259.


